2026 Author: Priscilla Miln | miln@babymagazinclub.com. Last modified: 2025-01-22 17:55:16
Rubella is a common childhood disease. What can it threaten during pregnancy? The statistics are staggering. Congenital rubella syndrome in newborn babies occurs annually. Up to 300,000 babies are born with this diagnosis. In the Russian Federation, 1/6 of all children with defects in appearance are deformities obtained under the influence of rubella on pregnancy. The consequences of this disease are terrible. And the saddest thing is that the standard symptoms in a sick person may not be observed at all. Rubella (Rubella virus) is transmitted to children between the ages of 3 and 9 years. The disease is characterized by a small rash all over the body and inflammation of the lymph nodes in the neck (often closer to the back of the head).

Rubella in pregnant women
Complications that a girl may face if she is not immune from rubella during pregnancy are determined by the following factors:
- The virus, infecting the blood cells of a woman, sneaks into the placenta. Thus, the fetus is under serious threat, the probability of malformations is high.
- A sixth of first trimester miscarriages and stillbirths are due to this disease in a woman.
- Even after birth, the rubella virus lives in the child's body for two years. Accordingly, he can infect someone around him. The risk remains even if the baby has developed antibodies in the blood.
Danger
The results and effects of rubella in pregnant women are unpredictable. The virus is spread by airborne droplets from an infected person. Subsequently, the sick mother passes the rubella to the child in the womb.
Through the air, the virus instantly spreads in the team. To prevent this disease, it is necessary to refrain from prolonged contact with the carrier. Chickenpox and measles, for example, are transmitted much faster.
Penetrating through the placenta into the baby's blood, the virus destroys cells that are just beginning to form. The genetic material is destroyed. If the pregnant woman is in the 3rd or 4th week, in almost 90% of cases a baby is born with defects in appearance. If a baby is born with this disease, he will transmit the virus through secretions and mucous membranes. The mother herself transmits the virus further, even before the onset of external manifestations of the disease.

Symptoms
The form of the disease exists in three types: standard, atypical (there are no rashes onbody) and asymptomatic. And most often rubella occurs without symptoms (90% of cases). It can only be detected by passing the appropriate tests.
What are the symptoms of rubella during pregnancy in women? These include:
- The period of manifestation of the disease (incubation) is from 11 to 24 days. Viral cells settle in the upper respiratory tract and begin to multiply actively. The lymph nodes on the head, usually closer to the back of the head, are affected. They swell and become the size of an average pea. They can be felt through the skin, when pressed, pain is felt. The longer the disease passes, the smaller the lymph nodes become.
- Severe course of the disease is accompanied by a high temperature (from 39 degrees). The woman's body aches and her head hurts, the need for food disappears.
- The vessels of the eyeballs swell, there is a slight swelling of the eyelids.
- Small red rash all over the body. Has the property of "combining" and forming large spots.
- As a consequence, inflammation of the joints and joint pain are often expressed.
At the first signs, a woman may think that she has a common SARS. But even in this case, it is important to remember that the drugs that you usually take are not recommended for use during pregnancy. Carefully study the instructions for the drugs, from which "Biseptol", "Co-trimoxazole" and other drugs. Pay attention to contraindications.
Consequences for the mother
Transferred rubella during pregnancy in the first trimester leads to defects in the appearance of the fetus. Bystatistics, such consequences come in 50-85% of cases. Babies show external deformities, problems with the eyes or hearing function. For a pregnant woman, rubella is dangerous because with prolonged undermining of immunity, diseases of the upper respiratory tract and lung diseases (otitis media, bronchitis, pneumonia, etc.) develop. After the rash appears within a month, arthritis or artlargia may appear. The upper limbs suffer, sometimes the knees. A rare consequence of rubella during pregnancy is meningitis or encephalitis.

Fetal infection
In the early stages of pregnancy, when all the systems of the child's body are laid down, rubella affects the cells of the growing embryo in the most detrimental way. Cell division slows down, the development of organs, the formation of the main vital systems of the fetus stops. In early pregnancy with rubella, the consequences in the form of spontaneous miscarriage are up to 40% of cases. 1/5 of babies are born dead. Up to 25% are cases of early death of children. The acute period of exposure to the embryo passes until the 12th week of pregnancy, later the risk of malformations in the child becomes lower, but the risk remains until the end of the third trimester.
When viruses in the mother's body pass into the bloodstream, they gradually penetrate into the epidermis of the uterus. The process of infection of the embryo begins about a week before a rash appears on the skin of a pregnant woman. Virus-infected cells attack the epithelium of the placenta, then move into the vascular systemembryo. Rubella infection during pregnancy for the fetus is manifested by dysfunction of vital systems and congenital external defects of the infant. This happens because the virus slows down the growth of embryonic cells, this interferes with the full development of the future human body. In relation to vital systems, the virus manifests itself only during the formation of hearing and vision. The consequences of rubella during pregnancy are often deafness or cataracts in the baby.
Consequences for the baby
Congenital rubella syndrome (CRS) was first described in 1941. The Austrian scientist N. Gregg recorded anomalies in children whose mothers had rubella during gestation. Over time, the list of consequences of rubella during pregnancy has been supplemented.
On what terms the development of anomalies was recorded:
- From the 3rd to the 11th week of pregnancy, the nervous system of the embryo suffers. From the 4th to the 7th week, the heart of the fetus and vision are under attack. More than half of fetal defects develop between the 3rd and 4th weeks of pregnancy.
- From the 7th to the 12th week, the auditory system suffers. The probability of a congenital disease is already falling here and is 15% of the number of cases.
- From the 13th to the 16th week, the probability of developmental defects drops even lower to 7%.
Which defects are related to ICS:
- Defects of the heart muscle (non-occlusion of the ductus arteriosus, ventricular septal defect, pulmonary stenosis).
- Vision defects (cataract, glaucoma, retinopathy, corneal clouding, chorioretinitis).
- Lack of abilityhear.
- Defects in the development of the nervous system are characterized by an incorrectly formed skull. The brain suffers, microcephaly develops. The consequence of rubella in pregnant women is the mental disability of the born child.
- Hypotrophy - delayed intrauterine development of the fetus.
- Defects in the development of the child's organs. Enlarged liver and spleen, dermatitis, bone infection, myocarditis, etc.
- Later, when the child grows up, the manifestation of diabetes mellitus, inflammation of the thyroid tissue, panencephalitis is likely.
- Rarely there are defects in the bones of the cranium. Sometimes the skeleton, organs of the genitourinary system and the digestive tract suffer.

How to find out about the disease?
Medicine has achieved excellent results in this matter. You can recognize the disease at any stage of its development. This will solve the problem of the spread of rubella among others, and take measures to alleviate the patient's condition. The serological method of research is considered the most effective analysis for rubella during pregnancy. Diagnosis is based on history and analysis of blood cells for antibodies.
How do antibodies work?
When a girl during the first weeks of pregnancy or planning cannot remember whether she was vaccinated against rubella, a blood sample is taken to check for the presence of antibodies. A fetal blood test is also performed. If those are found in the body of the expectant mother, then they penetrate to the babythrough the placenta and protect it from infection. When a child is born, antibodies enter the body through breast milk. Until the age of one, the child needs protection from this disease to prevent malformations.
Contact between a pregnant woman and an infected person
What should I do if a woman has rubella during pregnancy? The first step is to take a blood test to detect antibodies. If a woman has previously been vaccinated or has had a disease, then the tests will detect the presence of protection in the blood against re-infection. If such antibodies are not detected, the analysis is repeated after a month. If the result is positive (detection of rubella in a pregnant woman), it is recommended to terminate the pregnancy.
If the analysis is still negative, then the blood sampling will be repeated in another month. And if the presence of rubella in a pregnant woman is not confirmed, then the child can be saved. If the infection occurred later, at the 14th week or more, then the issue of termination of pregnancy is decided at the consultation.

How to treat?
Treatment of the disease is to eliminate its symptoms. It is necessary to lower the temperature, relieve rashes. Medical treatment of the focus of the disease by specialists has not yet been developed. Immunoglobulin (a substance containing antibodies) is not recommended to be injected into the blood. Perhaps only if the woman decided to leave the child. The standard treatment is bed rest, plenty of fluids, fever-reducing medications, and vitamin supplements. It is important to know that the receptionantibiotics and anti-infective agents (including "Analgin", "Biseptol") during pregnancy is contraindicated.
Vaccination
To minimize the risk of getting rubella during pregnancy, vaccination is recommended two months before conception. Thus, antibodies will have time to form in the body that will protect the fetus, and the mother, in case of infection, will tolerate rubella much more easily. For this, the Rudivax vaccine is used.
Monovaccine is injected into the shoulder muscle, its volume is 0.5 ml. Protective antibodies appear in the body after two to three weeks and persist for up to 25 years. During pregnancy, vaccination is prohibited. According to the results of studies in women who are not aware of pregnancy and have been vaccinated, infection of the fetus has been recorded. But no consequences on its development were found. After an accidental rubella injection, pregnancy can be saved. After childbirth, vaccination can be carried out after the examination. There is no rubella booster before pregnancy.

The consequences of vaccination
If you get vaccinated before pregnancy, the following consequences for a woman are possible:
- Reactions to the vaccine usually do not happen.
- If there is a reaction, then in the form of general malaise, slight fever, swollen lymph nodes on the back of the neck.
- Manifestations of arthritis are recorded in young women. Symptoms are observed a week after vaccination or a little later.
Otherthe consequences are associated with incorrect administration of the drug (overdose, violations of the rules of antiseptics, etc.).
How to prevent disease? Doctors' recommendations
Complex vaccination against rubella, measles and mumps is carried out at a young age. The first vaccination is given at 1 year, reactivation is carried out at 6 years. Girls and women during pregnancy planning can be re-vaccinated to avoid infection after conception. If vaccination has not been made, precautions are recommended. In case of illness or symptoms in the environment, it is necessary to isolate immediately. Communication with an infected person must be stopped for at least 10 days.
Pregnant women are advised to limit their stay in public places, especially in places where children gather. Many mothers with an older child are concerned about the question of what to do if he is ill with rubella. A pregnant woman will have to leave the child for a while, as the risk of infection is high. The minimum period for which communication should be interrupted is 5 days. At this time, care for the child will have to be transferred to someone from close people.
It is important to remember that rubella in a child is also treated by eliminating external signs of the disease (antipyretics, bed rest, etc.). It is contraindicated to take such drugs as Bactrin, Biseptol. What these drugs help with is not related to the manifestations of rubella in the child.

In closing
Disputes aboutthe advisability of vaccination. The issue is raised both in the context of childhood vaccinations and adults. With regards to rubella, the answer is obvious. To limit the risk of severe transmission of the disease in adulthood, especially for girls, doctors recommend vaccinating rubella. In the event of a categorical refusal to vaccinate, parents can help ensure that the child has experienced the disease at preschool age.
To do this, you can keep in touch with sick friends, for example. Thus, the child will become infected with rubella and will be ill with it in childhood. Antibodies to the disease will form in his blood, which will give immunity for the next two decades. In this case, the risks of rubella during pregnancy are minimized in girls in the future, and the consequences for the fetus will not be critical.
Recommended:
Hypertension during pregnancy: causes, symptoms, prescribed treatment, possible risks and consequences

Many women have heard of hypertension during pregnancy. In particular, those mothers who carried more than one child under their hearts know exactly what they are talking about. But at the same time, not everyone knows about the serious consequences, if you ignore the first alarming "bells" of this problem. But this phenomenon is not so rare among pregnant women. And so it can be considered a problem
Pharyngitis during pregnancy: symptoms, treatment methods and consequences

Pharyngitis is a rather serious disease that causes inflammation of the mucous membrane of the pharynx. Almost always, the disease requires treatment with medicines, in particular antibiotics. Therefore, women have a question about how to treat pharyngitis during pregnancy without harming the unborn baby
Hemorrhoids during pregnancy: symptoms, treatment and consequences
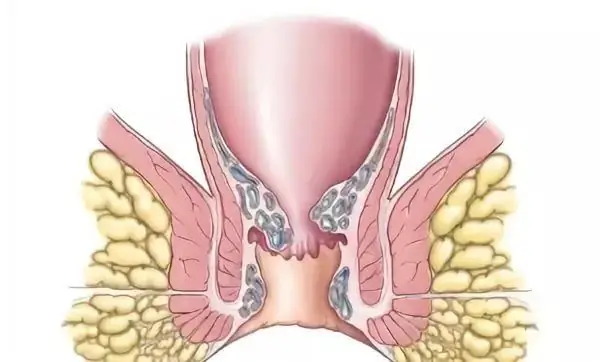
According to statistics, every third woman consults a doctor with a problem of hemorrhoids during pregnancy. Contrary to popular belief, the disease is not a normal physiological process during childbearing. This is a disease that requires an integrated therapeutic approach, otherwise serious consequences cannot be avoided
Hypotension during pregnancy: possible causes, symptoms, treatment, normal pressure during pregnancy, advice and recommendations from a gynecologist

What is hypotension during pregnancy? Is it a simple ailment, or a severe pathology that requires immediate medical attention? That is what we will talk about today. During the period of bearing a baby, every woman is faced with various ailments, because the body works "in three shifts", and gets tired in order. At this time, chronic diseases are exacerbated, and "sleeping" ailments are awakened, which could not be suspected before pregnancy
Increased bilirubin during pregnancy: norm, causes and symptoms, treatment, consequences

The state of a woman's he alth directly affects the course of pregnancy and the outcome of childbirth. Systematic analyzes and examinations throughout the entire period of gestation allow for constant monitoring of indicators in order to respond in a timely manner to identified deviations from the norm, if necessary. One of the methods for diagnosing the condition of a pregnant woman is a biochemical blood test. It is he who allows you to diagnose elevated bilirubin during pregnancy

